Nigerian medical personnel exodus to seek greener pastures overseas, coupled with insufficient specialists both for rural and urban services, pose serious threats to the country’s sustainable health care delivery. To worsen matters, there is also a large pool of unemployed medical personnel.
Statistics show there is one doctor to 6, 400 patients in Nigeria, a ratio which falls short of the World Health Organization standard of one doctor to 600 patients. To meet WHO’s benchmark, Nigeria needs to have 283, 333 doctors, measuring by a 170 million population base.
This means that the country needs 283, 308 additional doctors. In the USA and United Kingdom, it is said to be one doctor to 100 people. Malaysia is training 3, 500 doctors annually and ramping up to attain 1:600 by 2015 and 1:400 by 2020, which will exceed WHO’s recommendation.
Drawing inferences from what obtains in other countries, participants at a recent international health summit in Abia State, expressed concern over situation militating against effective health delivery in the state. The State’s Health Commissioner, Dr. Okechukwu Ogah, noted that human resources for health are critical for optimal health care delivery, especially at the grassroots.
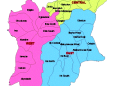
Dr. Ogah also disclosed that since its inception, the Medical Council of Nigeria, a total of 65, 759 medical doctors have been registered, translating to 38.9 per cent doctors per 100, 000 population or one doctor to 2, 572 patients. Unfortunately, only 25, 000 of them are practicing in the country. Worse still, these doctors are not evenly distributed within the country. Thus there are six doctors to 100, 000 in Zamfara, 50 to 100, 000 in Abuja, and six to 100, 000 in Abia.
A yawning gap exists between the rural and urban areas in terms of availability of medical personnel. But the similarity is that many states are in dire need of specialists in paediatrics, oncology, neurology and psychiatry among others. Despite rising cases of cancer, Nigeria has only 25 consultant oncologists who can only be accessed in seven states of Lagos, Oyo, Kaduna, Edo, Ondo, Sokoto, and Abuja. There are 50 neurologists and 40 neurosurgeons, doctors who specialize in the diagnosis and treatment of conditions affecting the nervous system.
The doctor-to-patient ratio is one neurologist to 3 million Nigerians with most of them urban based. No podiatrist, four forensic pathologists, only one diagnostic centre geriatrics in the country (University College Hospital, Ibadan), 600 consultant paediatricians to care for 700 million children. Hence people travel long distances within the country in search of specialists.
Ironically, while there is an inadequacy of some sort in number of health workers, on one hand, there is yet unemployment of trained medical personnel, on the other hand.
Glaring as this paradox is, it is a sorry situation for a country that has serious health care challenges as a huge proportion of the population has no access to qualified health personnel and are thus dying indiscriminately from treatable diseases. Dearth of health personnel is more pervasive in the North than in the South. Simplistic as this may sound, the truth of the matter is that highly trained health personnel are leaving in droves for greener pastures abroad.
America, Europe and the Middle East countries have high populations of Nigerian doctors, nurses and other health professionals. In fact, Nigeria is one of the several major health-staffexporting countries in Africa. The poor state of Nigeria’s health care system experts say, are traceable to several factors especially gross underfunding and shortage of skilled medical personnel at the primary health care level, obsolete equipment, and poor remuneration. The so-called intractable problem of poor electricity supply is sufficient disincentive for many while corruption in the system and the unstable polity contribute towards the drain of the nation’s human resources.
It is unfortunate that this has become the norm in this age and time. Unfortunately, medical tourism, which requires highly skilled specialists currently estimated to be a multibillion dollar industry, is ignored by health authorities. What Nigeria fails to understand is the changing face of medical tourism as many countries are now developing their health care sectors to meet local and international demands to attract foreign exchange.
At least, it is believed that the population of people that can pay for sophisticated medical procedures is growing and as such the country needs to develop on priority basis high-tech medicine such as well-equipped ICU, cardiac bypass surgery, organ transplant, advanced imaging technologies (MRI, PET), prenatal diagnosis, neo-natal screening, in vitro fertilization (IVF), among others.
Primary health care provisioning goes beyond structures or provisions of equipment and laboratory facilities, adequate qualified staffing because continuous improvement in orientation of health care services are equally important.
Federal and state governments should increase budgetary allocation for residency programme of young doctors, improve salaries and welfare packages, make rural areas attractive and conducive by providing good road network or connectivity to make those that are qualified stay in the country.
Governments can engage health institutions and associations to work out modalities for well-developed training and retraining programmes to encourage specialization to ensure that the standard that is obtainable here approximates what is available abroad to check the influx of people embarking on medical tourism.